Bacteria are often thought of as microorganisms that can cause disease. However, our bodies are full of bacteria, both ‘good’ and ‘bad’. Probiotics contain live bacteria and yeast which have been found to be beneficial to health, especially the digestive system. Probiotics are often referred to as ‘good’ bacteria, because they help keep the gut healthy and are believed to contribute to total wellness. Their efficacy has been demonstrated in a number of areas including diarrhoea, reduction of antibiotic-associated side effects, food allergies and lactose intolerance, irritable bowel syndrome, inflammatory bowel disease, oral and dental conditions. Moreover, use of probiotics has been associated with skin health and the improvement of certain skin disorders.
ORAL INTAKE
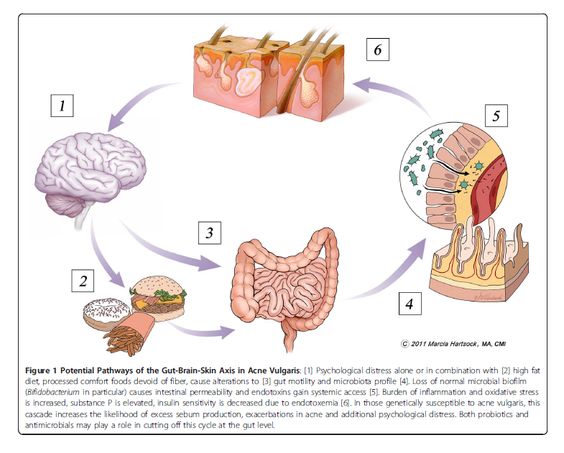
Several studies have looked at the effects of oral intake of probiotics on certain skin diseases. It has been suggested that probiotics may influence skin conditions such as acne and rosacea by affecting what is known as the “gut-brain-skin axis.” According to this theory, stress or anxiety alone or in combination with eating processed comfort foods that lack dietary fibre can slow digestion. This in turn changes the type and number of bacteria that live in the gut to ‘unhealthy’ bacteria. Eventually the gut lining becomes leaky and toxins are released into the bloodstream causing inflammation throughout the body. People who are predisposed to acne or rosacea can experience flares as a result of this shift in gut bacteria and subsequent inflammation. To counteract flares of acne or rosacea associated with the “gut-brain-skin axis,” it has been suggested that patients should find ways to help manage or cope with stress, change their diet or introduce ‘healthy’ bacteria to the gut in the form of probiotics. The probiotics will line the gut and create a ‘healthy’, sealed barrier that prevents inflammation reducing the incidence of acne or rosacea.
In 2014 Dr Whitney P. Bowe a dermatologist and spokesman for the American Academy of Dermatology said that “while more studies are needed to identify the most beneficial aspects of probiotics and determine whether topical or oral probiotics yield the best results, I think we can expect to see some cutting-edge probiotic products for acne and rosacea in the near future,”. He also recommended that in the meantime patients with acne or rosacea see their dermatologist to talk about adding foods with live active cultures, such as yoghurt, to their diets or taking an oral probiotic supplement daily. Although probiotics might not be a stand-alone treatment for acne or rosacea, he believes that they could be used as an effective combination therapy with prescription medications or over-the-counter topical treatments.
TOPICAL APPLICATION
Ceramides are lipid molecules that are found in high concentrations within cell membranes. In the top layer of the skin, ceramides hold skin cells together, forming a protective layer that plumps the skin and retains moisture. Their role has often been explained using a practical example where skin cells are referred to as the bricks and ceramides as the mortar. The effects of creams containing probiotics on skin ceramide levels have been investigated in a number of studies. One of the first in-vivo studies in healthy subjects found that topical application of a preparation containing probiotics (i.e. lactic acid bacterium Streptococcus thermophiles) led to increased stratum corneum ceramide levels. This increase was believed to possibly result in the improvement of the lipid barrier and a more effective resistance against abnormal skin dryness (xerosis).
A subsequent study involving subjects affected by atopic dermatitis (AD) was conducted to investigate the effects of a preparation containing probiotics on ceramide levels of the stratum corneum from AD patients. A reduced amount of total ceramides was thought to be responsible for functional abnormalities of the skin of AD patients. Two weeks application of the cream led to a significant and relevant increase of skin ceramide amounts as well as improvement of the signs and symptoms characteristic of AD skin (i.e. erythema, scaling, pruritus).
The demonstrated role of ceramides in both barrier and water-holding functions of healthy skin stratum corneum, suggested that the impairment of stratum corneum due to ageing or skin diseases could be caused by a ceramide deficiency. The effects of a cream containing probiotics were investigated in a study involving elderly women. Here again a statistically significant increase of ceramide levels in the stratum corneum was observed. Hydration was also higher compared to the area treated with Placebo. These results suggest that the experimental probiotic cream was able to improve the lipid barrier and to increase a resistance against ageing-associated xerosis.
The effects of topical application of probiotics have also been examined in skin affected with acne. Normal human skin can produce a range of antimicrobial chemicals that play an important part in eliminating potential cutaneous pathogens. Lactobacillus plantarum is a type of ‘good’ bacteria that produces antimicrobial peptide. When applied to the skin this probiotic can act like an anti-inflammatory but can also enhance the natural antimicrobial properties of the skin. Clinical studies were conducted to determine the effect of Lactobacillus extract on improvement of the skin barrier and reduction of erythema from chemical irritant, skin microflora, and acne. Results show that 5% of this probiotic was effective in reducing skin erythema, repairing skin barrier, reducing skin microflora, and exhibiting an effective reduction in acne lesion size.
PREVENTION
It has been suggested that over concern with high level of hygiene in western societies has caused a reduced microbial exposure in early life, which could be associated with the progressive increase in incidence of Atopic Dermatitis. The effect on AD of probiotics has been assessed in a study involving pregnant women who were given Lactobacillus GG, a probiotic that is safe to use in pregnant women and babies.
In a double-blind, randomised placebo-controlled trial Lactobacillus GG was given prenatally to mothers who had at least one first-degree relative (or partner) with atopic eczema, allergic rhinitis, or asthma, and postnatally for 6 months to their infants. The primary endpoint in this study was chronic recurring atopic eczema, which is the main sign of atopic disease in the first years of life. The results of the study showed that atopic eczema was diagnosed in 46 of 132 (35%) children aged 2 years. Asthma was diagnosed in six of these children and allergic rhinitis in one. The frequency of atopic eczema in the probiotic group was half that of the placebo group (15/64 [23%] vs 31/68 [46%]).Overall, the probiotic was found to be effective in prevention of early atopic disease in children at high risk. The persistence of the potential to prevent atopic eczema was further assessed once the children reached the age of 4 years. Atopic disease was diagnosed on the basis of a questionnaire and a clinical examination. 14 of 53 children receiving Lactobacillus had developed atopic eczema (26%), compared with 25 of 54 receiving placebo (46%). Results suggested that the preventive effect of Lactobacillus GG on atopic eczema extends beyond infancy.
PROBIOTICS IN DERMATOLOGY
Probiotics in the form of live microbial food supplements or topical preparations seem to hold several health benefits when administered in adequate amounts. We have talked about oral probiotics used to treat digestive problems as well as the broader use in skin as evidenced by “gut-brain-skin axis” theory first given 80 years ago. Details regarding use of probiotics for dermatological indications ranging from atopic dermatitis to acne and xerosis are evidenced in the scientific literature. Although some findings show no effect, an overview of scientific literature suggests that probiotic may have some therapeutic benefits for the skin and are safe to use. These initial results should encourage companies marketing probiotics to conduct more trials which include a larger population and are properly designed in order to validate the application of probiotics in prevention and treatment of skin diseases. As techniques emerge such as genetic profiling of the gut and skin microbiome, further research in this area will be possible.
REFERENCES
- Image Source: Copyright©2011 Bowe and Logan; licensee BioMed Central Ltd from Whitney P Bowe and Alan C Logan Acne vulgaris, probiotics and the gut-brain-skin axis – back to the future? Gut Pathogens 20113:1
- http://www.worldhealth.net/news/probiotics-skin-health/
- Bowe W, Patel NB, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis: from anecdote to translational medicine. Benef Microbes. 2014;5(2):185-99.
- Parodi A, Paolino S, Greco A, et al. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008;6(7):759-64.
- Muizzuddin N, Maher W, Sullivan M, Schnittger S, Mammone T. Physiological effect of a probiotic on skin. J Cosmet Sci. 2012;63(6):385-95.
- Di marzio L, Cinque B, De simone C, Cifone MG. Effect of the lactic acid bacterium Streptococcus thermophilus on ceramide levels in human keratinocytes in vitro and stratum corneum in vivo. J Invest Dermatol. 1999;113(1):98-106.
- Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet. 2001;357(9262):1076-9.
- Van der aa LB, Heymans HS, Van aalderen WM, Sprikkelman AB. Probiotics and prebiotics in atopic dermatitis: review of the theoretical background and clinical evidence. Pediatr Allergy Immunol. 2010;21(2 Pt 2):e355-67.
- Di marzio L, Centi C, Cinque B, et al. Effect of the lactic acid bacterium Streptococcus thermophilus on stratum corneum ceramide levels and signs and symptoms of atopic dermatitis patients. Exp Dermatol. 2003;12(5):615-20.
- Di marzio L, Cinque B, Cupelli F, De simone C, Cifone MG, Giuliani M. Increase of skin-ceramide levels in aged subjects following a short-term topical application of bacterial sphingomyelinase from Streptococcus thermophilus. Int J Immunopathol Pharmacol. 2008;21(1):137-43.
- Kumar S, Mahajan BB, Kamra N. Future perspective of probiotics in dermatology: an old wine in new bottle. Dermatol Online J. 2014;20(9).
- https://www.aad.org/media/news-releases/could-probiotics-be-the-next-big-thing-in-acne-and-rosacea-treatments