What is hyperpigmentation?
Our skin colour is determined by the number of pigment-producing cells called melanocytes in our skin. When an excessive or abnormal amount of melanin is produced and deposited by these cells, hyperpigmentation can occur. Hyper (i.e. over excessive) skin pigmentation is usually harmless, and appears as blotchy areas of the skin that are darker than their surroundings. A variety of factors can influence the development of hyperpigmentation including age, sun exposure, skin disease, and genetic disposition.
Skin hyperpigmentation can affect all skin phototypes, from very fair to very dark skin, and it is one of the top cosmetic skin concerns both in Australia and globally. As a result, many beauty brands have responded to consumer demand with a range of possible solutions that may assist with issues related to pigmentation in the skin. Note that skin blemishes due to other reasons, such as raised pigmented lesions, moles or skin cancers, will require a different approach.
Types of hyperpigmentation
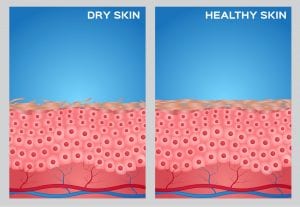
There are several different types of hyperpigmentation, which are categorised according to the depth of pigmentation in the skin.
Epidermal (superficial) pigmentation is usually close to the surface of the skin and is caused by sun exposure. This includes solar lentigos, freckles, and café au lait spots/macules.
Dermal (deep) pigmentation is normally located in the dermal layers. Examples are Hori’s macules and naevus of Ota.
Mixed dermal/epidermal pigmentation can be found in both the superficial and deeper layers of the skin. An example of this is Melasma.
Main causes
The production of melanin is a natural protective mechanism of the skin that is typically dependent on UV or sun exposure. This is distinct from excess production of melanin leading to darker spots of pigmentation in the skin. Hyperpigmentation has been associated with several causes:
- UV radiation
Most commonly, in geographical areas of high UV radiation levels (such as Australia), issues related to skin pigmentation are due to excessive UV or sun exposure. This is considered the most avoidable risk factor.
- Hormonal
Hyperpigmentation can be a result of hormonal changes during pregnancy. In some women, skin pigment may fade after delivery. Other causes are hormone treatments such as oral contraceptive pills containing oestrogen and/or progesterone, hormone replacement, intrauterine devices and implants. Examples of hormonal-induced pigmentation are melasma or chloasma.
- Trauma to the skin
Also known as post-inflammatory hyperpigmentation, this can be a result of acne or other physical trauma to the skin such as chemical peels or laser treatments.
- Birthmarks and acquired pigmentation
Congenital melanocytic naevus, café au lait spots, spilus naevus, Hori’s macules, and naevus of Ota are some examples.
- Medications and other products
Certain medications, as well as various toiletries and cosmetics may cause a phototoxic reaction that increases the risk of developing long term melasma.
Treatment
The main two types of treatments for hyperpigmentation are lasers and topical lightening products (e.g. creams). Some lasers used by experienced laser dermatologists have shown to produce fast and effective results. However, the cost, downtime (i.e. recovery post-treatment), risks associated with lasers such as worsening of the pigmentation, loss of normal skin pigmentation (hypopigmentation) or scarring of the skin, need to be taken into consideration. On the other hand, topical skin lightening products may not remove the pigmentation completely, but have shown to be effective at lightening the colour of hyperpigmentation, reducing its appearance.
Topical skin lightening preparations
A number of topical ingredients have shown to be helpful in reducing the appearance of hyperpigmentation. Inhibiting enzymes that produce melanin and increasing the turnover of the skin (i.e. exfoliation) are two methods that can be used to fade existing pigmentation. Common lightening agents include: hydroquinone (in Australia, this requires a doctor’s prescription), arbutin, retinoids, glycolic acid, lactic acid, licorice, kojic acid, paper mulberry bark extract, niacinamide, and vitamin C.
However, the first line of treatment for hyperpigmentation is unanimously recommended by dermatologists and skin care professionals. This is the consistent daily application of sunscreen on the areas predominantly affected by hyperpigmentation, such as the face. Sunscreen serves to avoid worsening of the existing pigmentation, to prevent the appearance of new pigmentation, and to maximise the effect of any skin lightening products being used.
A shift has been noted in recent years from sunscreens being used to protect from UV during outdoors activities, to sunscreens being used as an everyday anti-ageing product. This is even more so for people affected by hyperpigmentation. It is recommended for one to apply sunscreen even if it is cloudy, and even if they are in a car or building, as UV light can penetrate windows. Avoiding direct sunlight on the face is important for people affected by hyperpigmentation, especially around midday when the UV index is highest. Naturally, it is also recommended to wear a hat and seek the shade when outdoors.
Studies on cosmetic products to improve the appearance of hyperpigmentation have shown good results when the application of these products was consistent and supported by regular UV and sun protection of the area(s) exhibiting the hyperpigmentation. More of such in vivo studies need to be conducted on existing and newly developed products claiming an effect on skin hyperpigmentation in order to prove their efficacy.
References:
https://www.thevictoriancosmeticinstitute.com.au/detail/skin-pigmentation-treatment/